Perspectives combines AI-powered utilization review with proactive chart auditing — built to maximize approved days of care and eliminate preventable denials.
Trusted by top behavioral health programs around the nation


















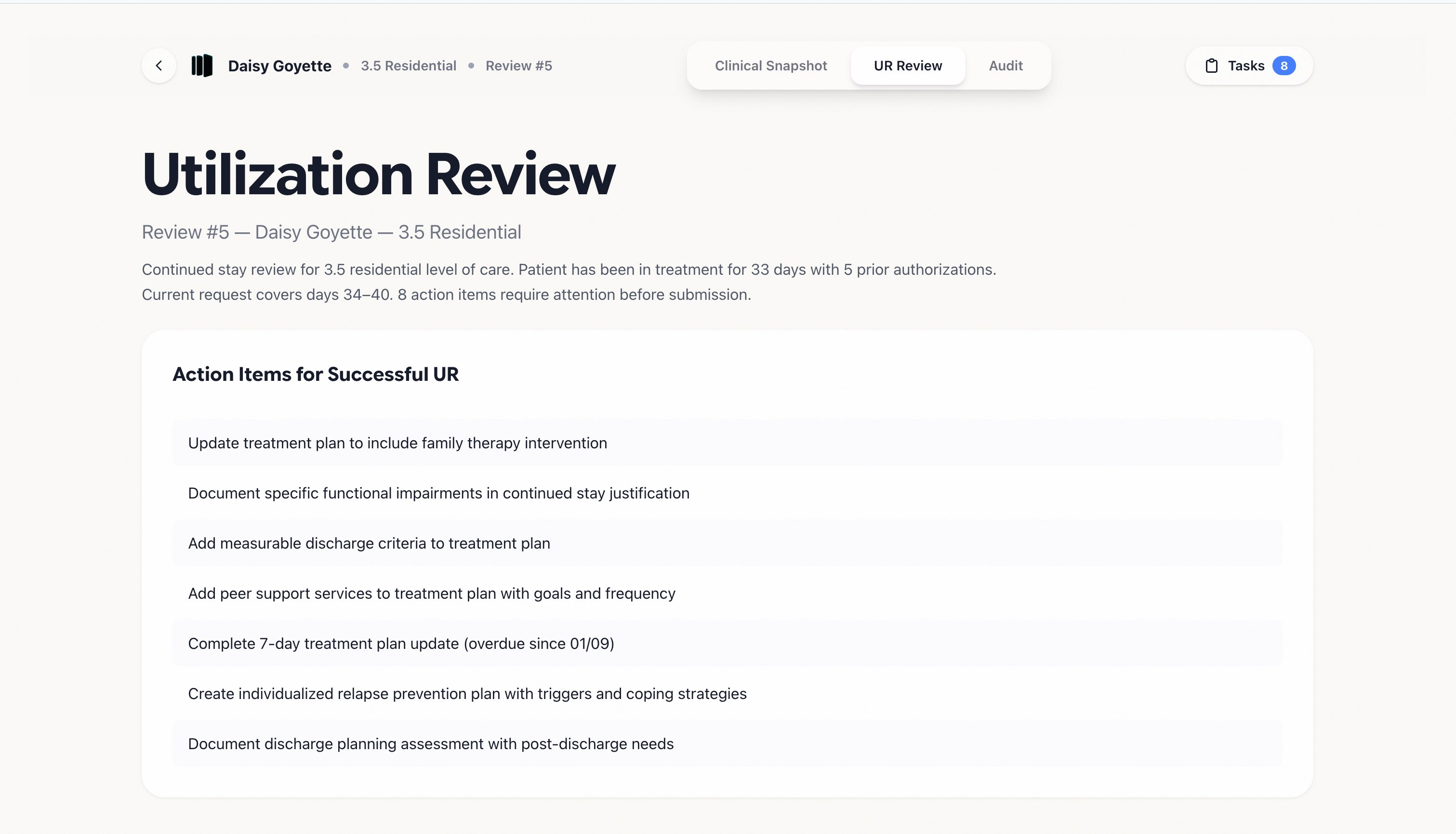
A system to increase approved lengths of stay, prevent payor-driven stepdowns, and protect against clawbacks.
Progress Note dated 01/11/2026 documents a Peer Support session. However, the current Treatment Plan does not list Peer Support as an intervention.
Psychosocial Assessment documents: "Mother and brother Devin identified as sober supports. Patient requests family involvement in treatment."
Patient admitted 01/02/2026. No discharge planning note found within 72 hours of admission as required. Most recent documentation is dated 01/08/2026.
Progress Note dated 01/09/2026 documents patient expressed passive suicidal ideation during group. No updated suicide risk assessment completed following this disclosure.
Current treatment plan lists "Patient will improve coping skills" as a goal. No measurable objective, baseline, or target date is documented for this or 3 other goals.
MAR shows patient has been on Naltrexone 50mg since admission on 01/02/2026. No medication education note found in the record documenting patient education on purpose, side effects, or interactions.
F10.20 · Alcohol use disorder, Severe
F12.20 · Cannabis use disorder, Moderate
F13.20 · Sedative use disorder, Severe
F12.20 · Cannabis use disorder, Moderate
F14.20 · Cocaine use disorder, Severe
F11.20 · Opioid use disorder, Severe
F10.20 · Alcohol use disorder, Severe
F15.20 · Stimulant use disorder, Moderate
PAWS symptoms present — headaches and migraines treated with PRN Ibuprofen. CIWA scores of 5 and 7 recorded on admission. Vitals 137/99, HR 75. UDS collected 02/04/2026 positive for Gabapentin, Lorazepam, Benzodiazepines, Buprenorphine, Opioids & Opiate Analogs.
Yes, the member has reported headaches and migraines, for which PRN medications specifically noted for PAWS (Ibuprofen) were administered. Additionally, CIWA scores of 5 and 7 were recorded on admission.
The provided documentation does not specifically mention PAWS (Post-Acute-Withdrawal Syndrome) symptoms or their impact on the client's participation in treatment.
137/99, 75
The last UDS was collected on 2026-02-04. Result: positive (detected: Gabapentin, Lorazepam, Benzodiazepines, Buprenorphine, Opioids & Opiate Analogs).
The pilot involves a short, hands-on rollout where we:
Yes. Reclaim works across all behavioral health EMRs, including Netsmart, myAvatar, Kipu, BestNotes, Alleva, and more.
Implementation is straightforward. We set it up with a single point of contact, align on your goals and criteria, and start producing usable outputs quickly.
Our goal is that implementation takes very little work on your end.
We're HIPAA and SOC 2 compliant, audited by a third party. Security documentation is available upon request.
Reclaim pulls every chart from the EMR and flags documentation gaps against Joint Commission requirements and payer-specific rulebooks — so your team knows what to fix before a reviewer ever sees it.
Learn moreReclaim reads the full clinical record and generates a complete UR packet in seconds — structured, cited, and optimized for approval. No more hours of manual write-ups.
Learn more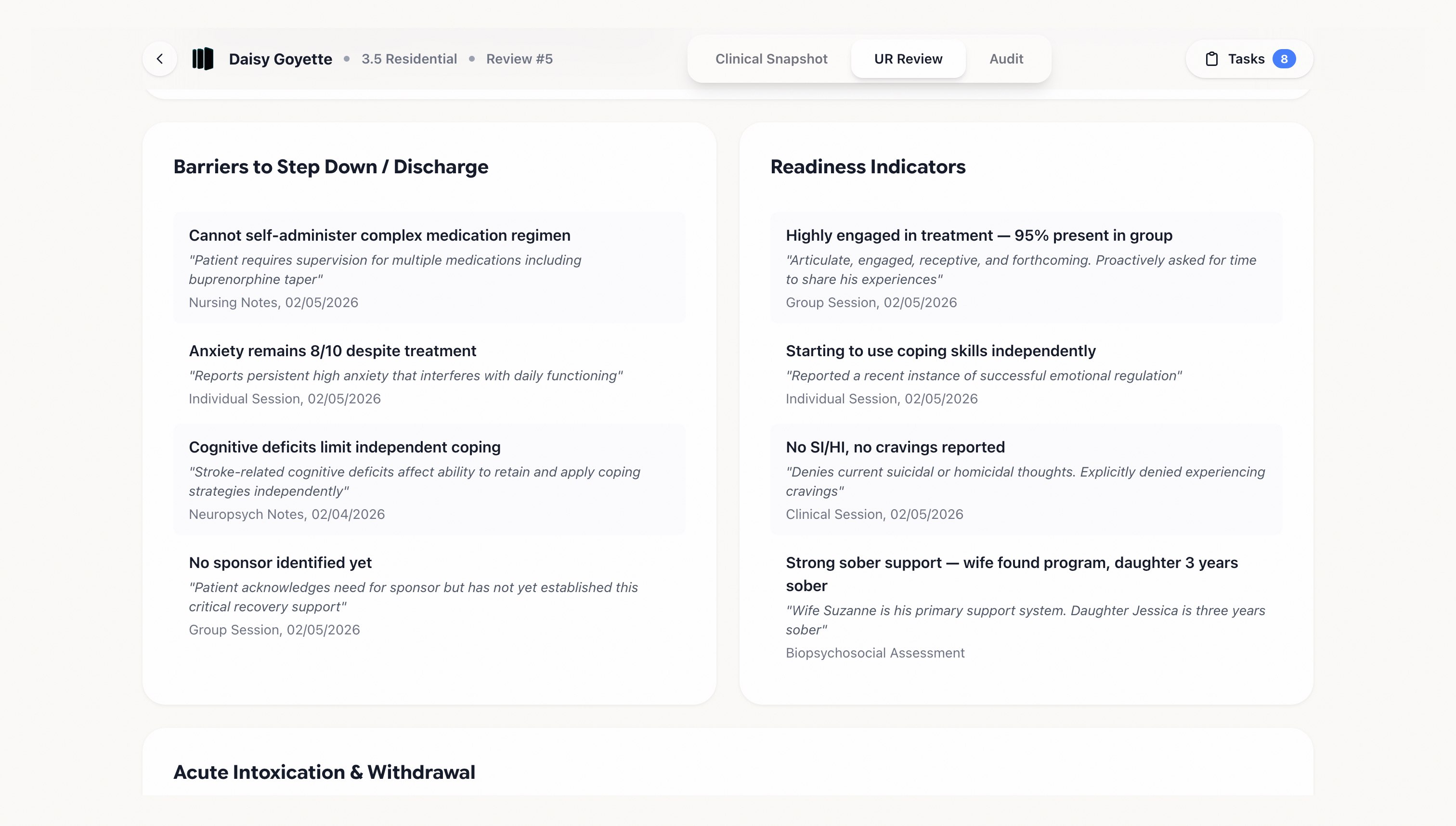
"I'm kind of a stickler on documentation. I just can't have it piling up. I was kind of hesitant at first and when I first started using I thought it was easy.
Now, I probably spend like 2 minutes on a note...my brain doesn't feel so tired"
The best behavioral health AI scribe on the market. Fills out entire assessments, biopsychosocials, or progress notes, with language optimized for JCO, CARF, and payer compliance.
Book a demo →